Abstract
Activated JAK2 signaling is a central feature of myeloproliferative neoplasm (MPN) pathogenesis, and drives myeloid blood cell production through constitutive activation of STAT transcription factors, the PI3K/AKT and the MAPK signaling pathways. JAK2 inhibitors show significant, but limited clinical efficacy such as seen for ruxolitinib, a type I JAK1/2 inhibitor approved for the treatment of myelofibrosis (MF) and polycythemia vera (PV). Given the impact of JAK2 inhibition on the MAPK signaling pathway in MPN has not been studied in vivo, we hypothesized that MAPK signaling could contribute to MPN cell survival in the setting of JAK kinase inhibition.
We observed that JAK2 inhibition by ruxolitinib and other agents suppressed phosphorylation of ERK1/2, the distal kinases in the MAPK pathway, in MPN cell lines. By contrast, these JAK2 inhibitors could not suppress MAPK signaling in vivo in Jak2 V617F- and MPL W515L-driven murine MPN models. In the in vivo setting, ERK remained fully activated despite JAK2 inhibition at therapeutic or higher doses suggesting that compensatory signaling may bypass JAK2 inhibition. E x vivo exposure of Jak2 V617F and MPL W515L primary mouse hematopoietic cells or PBMCs from JAK2 V617F mutant MPN patients to ruxolitinib demonstrated MAPK inhibition, indicating that cell extrinsic stimuli maintain ERK activation in vivo .
To identify secreted factors which could mediate JAK-independent ERK activation in vivo, we performed receptor tyrosine kinase arrays in Jak2 V617F and MPL W515L mouse splenocytes in presence and absence of ruxolitinib. This allowed us to show that expression and activation of PDGFRα was maintained in MPN cells upon JAK inhibitor treatment. Although the production of multiple cytokines was reduced by ruxolitinib, PDGFA and PDGFB production were not attenuated by JAK2 inhibitor treatment. We confirmed that PDGF-BB was present at higher levels than PDGF-AA in bone marrow supernatant, spleen supernatant and serum suggesting it is the primary ligand activating MAPK signaling through PDGFRα. Stimulation of primary Jak2 V617F bone marrow and spleen cells with PDGF-BB ex vivo induced ERK activation in presence of ruxolitinib suggesting PDGF-BB can mediate bypass ERK activation.
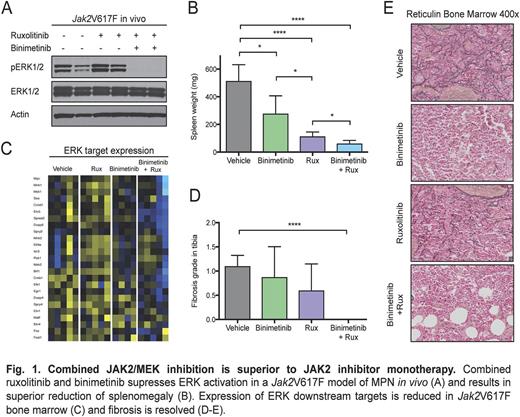
We next assessed the efficacy of combined JAK/MEK inhibition in vivo . Binimetinib, a clinical-grade MEK1/2 inhibitor, inhibited ERK phosphorylation in Jak2 V617F and MPL W515L murine models at a single dose or with extended treatment, and showed modest efficacy when given as monotherapy in vivo. Of note, dual targeting of JAK2 and MEK with combined ruxolitinib/binimetinib was superior to both single agent therapies. In the Jak2 V617F model of PV, dual JAK/MEK inhibition corrected splenomegaly and reduced the increased hematocrit, reticulocytes, erythroid and megakaryocytic-erythroid progenitor populations characteristic of this MPN model. Bone marrow and spleen fibrosis was resolved by dual JAK/MEK inhibition along with reduced bone marrow hypercellularity and decreased mutant allele burden. Expression of ERK downstream targets including ETV5, EGR1, CCND1, DUSP4, DUSP6 and SPRED2 was effectively reduced by combined JAK/MEK inhibitor therapy. Dual JAK/MEK inhibition with ruxolitinib/binimetinib also showed increased efficacy in the MPL W515L model of ET/MF with improved correction of leuko- and thrombocytosis, extramedullary hematopoiesis, hepato- and splenomegaly and megakaryocytic hyperplasia. Combined JAK/MEK inhibition with ruxolitinib/selumetinib showed similar effects. Importantly, dual JAK/MEK inhibition reversed fibrosis to an extent not seen with JAK inhibitor monotherapy.
Taken together, these data demonstrate that JAK2 inhibition incompletely suppresses ERK activation in MPN in vivo and that cell non-autonomous ERK activation through PDGFRα contributes to the limited efficacy of JAK inhibition in MPN. We show that dual targeting of JAK2 and MEK provides improved therapeutic efficacy by preventing bypass ERK activation and suggest that dual JAK/MEK inhibition should be pursued as a therapeutic approach for MPN patients. Our data also suggest that cell non-autonomous MAPK activation might represent a mechanism of resistance to targeted therapies which is only observed in the in vivo setting and which can guide combination therapy trials in different malignant contexts.
Radimerski:Novartis: Employment. Skoda:Novartis: Consultancy, Speakers Bureau; Shire: Speakers Bureau; Baxalta: Consultancy, Speakers Bureau. Levine:Roche: Research Funding; Celgene: Research Funding; Celgene: Research Funding; Roche: Research Funding; Qiagen: Equity Ownership; Qiagen: Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal